Depression
This information was obtained from credible government and private organizations and results from evidenced-based medicine; however, it is not meant to replace a medical or psychiatric professional’s advice. It was reviewed by a psychologist who is well-versed in this information and who treats many Veterans. It is current as of March 26, 2015.
What is depression?
Depression is caused by a variety of factors that contribute to developing and maintaining depressive symptoms. Depression is not about feeling blue or about the normal reactions we have to life events, such as losing a job, getting a divorce, or the death of a loved one, and specifically for Service members, depression is not about feeling sad and angry or fear and worry about adjusting to life post-deployment. These are reactions to normal life stressors. Instead depression occurs when these feelings and reactions are not normalized (resolved over a specified period of time). In addition, depression can develop out of the blue without an apparent cause.
 So, what exactly is depression? Depression is classified as a mood disorder wherein there is a persistent sense of sadness, discouragement, hopelessness, and loss of interest in regular activities and life in general that lasts for more than two weeks on most days. It affects how you feel, think, behave, and function, which leads to physical, emotional, behavioral, and psychological symptoms. Depression symptoms can range from the inability to do common everyday activities (e.g., going to work, taking care of family, even getting out of bed or maintaining proper hygiene) to feeling like life is not worth living. These symptoms can significantly impact your life and relationships. Depression may be a once in our lifetime experience, or there may be multiple episodes or recurrences.
So, what exactly is depression? Depression is classified as a mood disorder wherein there is a persistent sense of sadness, discouragement, hopelessness, and loss of interest in regular activities and life in general that lasts for more than two weeks on most days. It affects how you feel, think, behave, and function, which leads to physical, emotional, behavioral, and psychological symptoms. Depression symptoms can range from the inability to do common everyday activities (e.g., going to work, taking care of family, even getting out of bed or maintaining proper hygiene) to feeling like life is not worth living. These symptoms can significantly impact your life and relationships. Depression may be a once in our lifetime experience, or there may be multiple episodes or recurrences.
What is depression not? Depression is not something you can just “snap out” of and it is NOT a sign of weakness or character flaw. It is a medical condition that has effective treatments.
In approximately 50% of those diagnosed with depression, there is also a diagnosis of anxiety. Examples of anxiety disorders include general anxiety disorder (general feeling of anxiety), social anxiety disorder (anxiety experienced in social situations), panic disorder, obsessive-compulsive disorder, and Post Traumatic Stress Disorder (PTSD). Like depression, there are many treatment options for anxiety disorders, but remember that anxiety is a separate and distinct disorder with separate treatment options. Depression and anxiety can be treated at the same time.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the types of depression?
There are three major types of depression, which may or may not occur with an anxiety disorder;
Major Depressive Disorder (MDD): MDD is characterized by a variety of symptoms listed in the “what are the symptoms of depression” section and is classified as mild, moderate or severe depending on the number of symptoms and the degree of negative impact they have on a person’s daily activities and ability to cope. People must experience these symptoms most of the day on most days for at least two weeks. In general, MDD is disabling as it interferes with most daily activities. People can experience just one MDD episode in a lifetime or they may suffer from recurrences of MDD over their lifetime. Depression can also become chronic. Those experiencing MDD can be at greater risk for suicidal thoughts and behviors, especially as the degree of severity increases and when there is a history of suicidality and substance use, or comorbid diagnoses (e.g., substance use, TBI, PTSD). Although MDD and its effects sound dire, do not lose hope because there are evidence-based effective treatments that will help most MDD sufferers get better.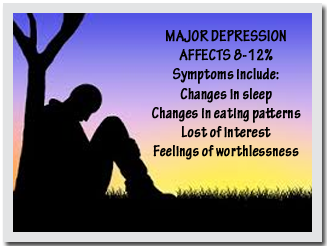
Persistent Depressive Disorder (PDD) aka dysthymia: PDD is a less severe form of MDD that generally lasts at least two years. Although, it has the same symptoms as MDD the following symptoms—low energy, poor appetite or eating too much, and oversleeping or trouble sleeping.—are more prevalent and symptoms manifest themselves mostly as increased stress, irritability, and inability to derive pleasure from usual activities. PDD sufferers can experience one or more episodes of MDD, but like MDD, there are evidence-based effective treatments that will help most PDD sufferers get better.
Minor depression fulfills the time frame for MDD in that symptoms last two weeks or longer; however, the number of symptoms does not fulfill the criteria for a full MDD diagnosis or they may be atypical (not the norm). Those with minor depression have a high risk of developing MDD without treatment. Some minor depressions manifest themselves in different forms, for example, Seasonal affective disorder (SAD).
Seasonal affective disorder (SAD): This type of depression occurs during specific times of the year. Most cases occur during the fall and winter. Presently, the scientific world attributes this to the lack of light during these months. This is supported by the fact that people in northern climates have a higher incidence of SAD. Those of you stationed in the far north, (e.g., Alaska) may experience SAD. Light therapy has been shown as an effective treatment; the military has used light therapy for Soldiers in Alaska. SAD in the spring and summer has been diagnosed, but much less so.
Other minor depressions include psychotic depression and postpartum depression.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the risk factors for and causes of depression?
Risk factors: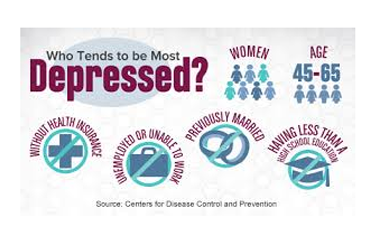
- Social isolation
- Chronic pain
- Chronic sleep issues
- Excessive Alcohol Use or Substance use
- Gender (females > males)
- Individuals aged 45-64
- History of an anxiety disorder
- Previous episode of depression, especially if it started in childhood or as a teen
- Blood relatives with history of depression, bipolar disorder, substance use, and suicide
- Certain personality traits like low self-esteem, being overly dependent, self-critical or pessimistic, and rumination (constantly thinking about problems or negative situations)
- Friendships with those that overly focus on discussing problems (co-rumination)
- Stress or traumatic events (e.g., financial problems, relationship stress, parenting issues, deployment, extended separation from social supports, etc.)
- Socioeconomic risk factors (e.g., never married or divorced, no health insurance, unable to work or unemployed, those with less education, being poor)
- Co-morbid conditions (e.g., PTSD, TBI, chronic disease)
Causes:
Various websites list several causes for depression; however, current research indicates that depression is a disorder of the brain that mostly results from bio-physiological factors, including changes in brain structure, function (e.g., changes in brain chemistry), and hormone imbalances.
Biological: For those with depression, imaging tests show that there are physical changes to their brains that control mood, sleep, thinking, appetite, and behavior, the significance of which is under study. They are not used to diagnose depression.
Biochemical: The brain chemistry (aka neurotransmitters) is off-balance (e.g., there is not enough of them, they are broken down faster, or they are absorbed more quickly). Neurotransmitters serve as an important check and balance system within the brain, so if one is affected, the others do not function properly, resulting in more disorder. This alters communication between brain cells, which results in symptoms of depression. Scientists have associated serotonin and norepinephrine as the primary neurotransmitters associated with depression. Dopamine is implicated as well.
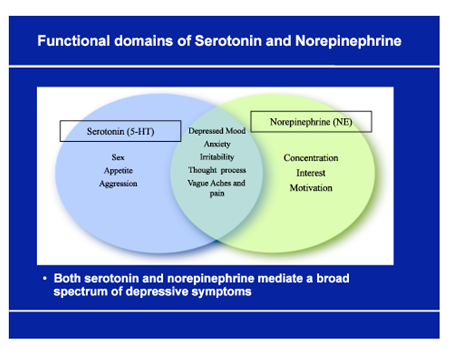 Serotonin affects sleep, memory, appetite and digestion, mood and social behavior, and sexual desire and function. Some symptoms resulting from decreased levels of serotonin are hostility, irritability, and suicidal ideation (thinking about committing suicide).
Serotonin affects sleep, memory, appetite and digestion, mood and social behavior, and sexual desire and function. Some symptoms resulting from decreased levels of serotonin are hostility, irritability, and suicidal ideation (thinking about committing suicide).- Norepinephrine also referred to as a stress hormone, is involved in triggering the “fight or flight” response to dangerous situations; it increases glucose, heart rate, breathing rate, and the amount of oxygen to our brains. Less norepinephrine causes dullness and lethargy (lack of energy or enthusiasm).
- Dopamine affects mood, sleep, learning, movement, attention, memory, pleasurable reward, and behavior and cognition (thinking). Less dopamine affects the ability to learn and pay attention, alters sleep patterns (too much or too little), decreases mood and memory, and stops us from being interested in and enjoying simple life pleasures.
In the "what are the symptoms of depression" section, you will be able to connect the functions of these neurotransmitters with the symptoms of depression.
Hormonal: Hormones, for example, thyroid hormones, directly affect the brain, which has many receptors for hormones. Hormones act on the brain by changing gene action, which changes both neuronal structure and function. This alters brain circuitry and neurotransmission of signals, which can cause many depressive symptoms. What this tells us is that any life event or environmental situation, such as increased stress from a trauma or natural disaster, changes hormonal function, which in turn affects brain structure and function. One result of these changes is depression.
Genetics: Scientists have linked genes with depression. If biological relatives suffer from depression, there is a greater chance that you will, too. Currently, scientists are trying to identify specific depression-related genes, and how they interact with the environment and other factors, and their role in causing depression. Hopefully, this will increase early detection and treatment, and in the future, involve gene therapy.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the symptoms of depression?
- Feeling sad, empty, tearful, or unhappy
- Feeling decreased pleasure or loss of interest in normal activities (inability to get enjoyment from things you once enjoyed)
- Feeling angry, irritable, and frustrated even about small problems
- Feeling anxious, agitated, or restless (e.g., worrying too much, unable to sit still)
- Feeling worthless, hopeless, persistently pessimistic, or guilty (e.g., constantly thinking about past failures and taking blame for things that you are not responsible for)
- Poor self-esteem and self-image
- Feeling tired or experiencing no energy (fatigue), such that the smallest tasks are hard to do and they require extra effort
- Decreased or loss of sex drive
- Having problems with sleep, getting too much or too little and early-morning wakefulness
- Experiencing changes in appetite, either eating too much or too little resulting in weight gain or loss
- Thinking, speaking, and moving more slowly
- Having trouble thinking, reasoning, concentrating, making decisions, and remembering things
- Experiencing physical symptoms that cannot be explained and do not respond to treatment (e.g., headaches, back pain, digestive problems, diffuse body pain)
- Frequently thinking about death and suicide, suicide attempt
Note:
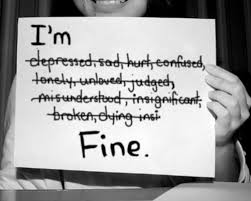
These symptoms can be so mild that the person experiencing them feels unhappy and miserable without understanding why and they may not be recognized by others. However, someone with minimal signs of depression can still be experiencing profound inner turmoil. In others, the symptoms are so severe that it is obvious to the person experiencing them as well as those around him or her that something is wrong.
Not every person with depression will have all of these symptoms; depression affects each person differently, and thus, symptoms can vary widely from person-to-person.
Quite often, depression does not go away by itself and oftentimes without treatment gets worse causing other health problems and interfering with other areas of life (e.g., job, relationships), and potentially leading to substance use and suicide. Although some who experience a situational depression can get better on their own once the situation resolves, for most with depression, treatment is the best option.
Sometimes people suffering from depression do not have the energy to seek out help. It is up to the people around them to help them seek out mental health services. Depression carries a higher risk of suicide, therefore suicidal thoughts or intentions should be taken very seriously. If that is the case staying with them and calling 911 or taking them to the nearest emergency room is paramount and may save their lives. The importance of getting help for someone you think is depressed and/or suicidal cannot be overemphasized!
People who are reluctant to seek out treatment should talk to someone they trust, such as a friend, family member, or faith leader. For those in the military, your chaplain offers a trusting and confidential environment.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
How is depression diagnosed?
The earlier depression is diagnosed the better because the earlier treatment begins the better the outcome. Part of the diagnostic process may involve using tests and exams to rule other other health problems that may be causing the same symptoms. A history and physical exam will gather information about your symptoms to rule out an underlying physical problem that may be causing symptoms of depression (e.g., thyroid disease that causes a hormonal imbalance that negatively affects brain structure and function). Lab tests can include a complete blood count, electrolytes, blood urea nitrogen, creatinine, toxicology screen, and in the case of suspected thyroid disease, thyroid function and hormone level tests. Imaging studies like CT and MRI scans are performed if an organic brain syndrome is suspected. Psychological exam via questionnaires and face-to-face interview are used to specifically evaluate symptoms, such as changes in thoughts, feelings, and behavior patterns. Tests include: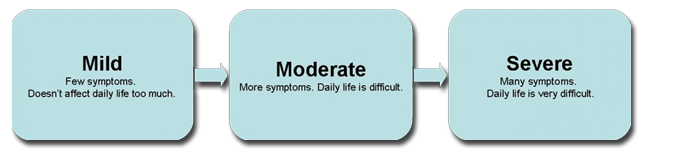
- Sung Self-Rating Depression Scale
- Beck Depression Inventory (BDI)
- Criteria for Epidemiologic Studies-Depression (CES-D) scale
There are specific criteria for a diagnosis of depression. Meeting this criteria requires that you experience symptoms most of the day, nearly everyday for at least two weeks. You must have at least one of the following symptoms (a) feeling sad, empty, tearful, or unhappy or (b) feeling decreased pleasure or loss of interest in normal activities, plus at least five other symptoms listed in the “what are the symptoms of depression” section.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
How is depression treated?
Those with severe symptoms may require both inpatient and outpatient treatment., whereas those with mild or moderate symptoms generally require outpatient treatment. Here is the good news; there are many treatment options to manage depression and anxiety that fall under four options: self-management, therapy, medication, and therapy with medication. So anyone who is diagnosed with depression and/or anxiety should not lose hope.
Self-management
There are steps you can take to empower yourself to manage your depression:
- Learn about depression. Knowledge is power and serves as a motivator to do what it takes to get well.
- Talk to your providers about treatment options, about what you are thinking, and about how you are feeling. Your treatment will progress more quickly if you are an active partner in treatment. You are the authority when it comes to how you are feeling. Your provider can only be as good as the information you provide to them.
- Stick to your treatment plan by attending all therapy sessions, taking medications as directed, and not stopping them abruptly. Even when you feel better you still need to maintain treatment until the agreed upon time. Stopping treatment too early can undo all the hard work you have just put in, and abruptly stopping medication can potentially lead to relapse.
- Pay attention to warning signs that symptoms are getting worse or that you feel suicidal.
- Exercise regularly, eat a nutritious diet, and get plenty of sleep (maintain regular schedule).
- Avoid alcohol and illicit drugs.
- Simplify your life and structure your time (e.g., set reasonable goals for what you can and cannot do; give yourself permission to do less when you are down).
- Do not isolate yourself; reach out to family and friends.
- Learn ways to relax and manage stress.
- Do not make important decisions when you are down as you may not be thinking clearly.
- Consider doing some type of volunteer activity. Creating meaningful ways to contribute helps keep depression at bay.
Therapy
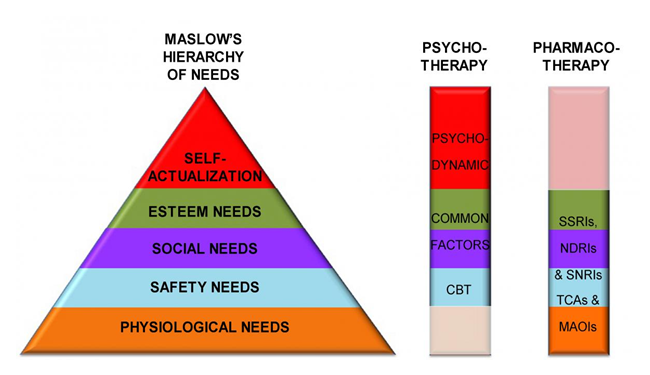
There are proven therapies that decrease depression symptoms, especially for mild and moderate depression. In fact, therapy may be the best option in this case. Therapy will focus on your concerns and how to effectively treat them. Sessions can be individual, group, family, and couple-oriented. You will generally have 8 to 20 sessions that last 45 to 60 minutes. Evidence-based medicine has identified several effective therapies: Psychodynamic Therapy, Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT), and Problem-Solving Therapy (PST).
Psychodynamic Therapy is talk therapy that uses open-ended and free association of ideas (you talk freely about what is bothering you) that will help you explore all of your emotions, especially those from the past and your unconscious mind. Psychodynamic Therapy will help you identify feelings you may not be aware of with the goal of helping you understand how the whole range of your emotions is affecting your present-day mood and behavior. You will also confront feelings you may be avoiding and develop the internal capacity and range of resources (coping mechanisms and support systems) to help you learn healthier ways to deal with life stressors and live a more fulfilling life. Sessions occur once per week for about 50 minutes. Psychodynamic Therapy tends to be more long term without a time limit, and therefore can last for over one year; however, there have been cases where therapy can end after 16- 20 weeks.
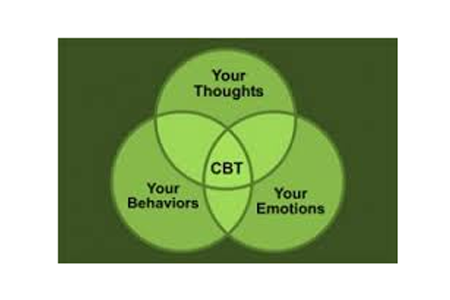 Cognitive Behavioral Therapy (CBT) is used to change negative thoughts, patterns, and behaviors by helping you interpret your environment and interactions with the people in your lives in more positive and realistic ways. CBT will help you learn new skills to mitigate these negative thoughts and behaviors, improve your mood, and increase your ability to handle stress. Therefore, the goal of CBT is to teach you strategies to create positive thoughts and behaviors by teaching you to recognize the thoughts and behaviors that are negatively affecting your life and replacing them with useful and beneficial thoughts and behaviors.
Cognitive Behavioral Therapy (CBT) is used to change negative thoughts, patterns, and behaviors by helping you interpret your environment and interactions with the people in your lives in more positive and realistic ways. CBT will help you learn new skills to mitigate these negative thoughts and behaviors, improve your mood, and increase your ability to handle stress. Therefore, the goal of CBT is to teach you strategies to create positive thoughts and behaviors by teaching you to recognize the thoughts and behaviors that are negatively affecting your life and replacing them with useful and beneficial thoughts and behaviors.
Interpersonal Therapy (IPT) is useful for those with relationship problems that may be contributing to depression symptoms, and making them worse. The goal of IPT is to reduce your symptoms of depression by solving problems you are experiencing in your relationships through teaching communication, conflict resolution, and problem-solving skills over 16-20 sessions. Research shows that IPT is effective for those with mild to moderate depression.
Problem-Solving Therapy (PST) is similar to IPT in that it teaches groups of people how to solve problems, reach set goals, and change negative behaviors. It is achieved though teaching you to see and understand how your problems are contributing to your depression and then uses step-by-step problem-solving techniques using six sessions over a three month period. Research shows that PST is effective for those with mild to moderate depression.
If your specific therapy does not result in improvement within six to 12 weeks, a different therapy or medications may be required.
Medications
There are several medications available that work to increase the levels of neurotransmitters. They take time to work; many can take at least four to six weeks, so it is important that you give your medications time to do their job. In addition, the first medication you try may not be the right one for you, so it is important to tell your physician whether or not your symptoms have decreased, and if you are experiencing side effects, so that the correct medication can be found. Since the goal is remission, you may have to try several medications before you find the right one. It may also take more than one medication to get the job done. You may have to take two antidepressants or you may be prescribed mood stabilizers, antipsychotics, and anti-anxiety and stimulant medications to take with your antidepressant based on your symptoms. It is very important that you take your medications consistently and that you do not stop treatment abruptly because you may experience sudden worsening of depression. In the long run, antidepressants reduce suicide risk; however, suicide risk may increase when starting an antidepressant, therefore, follow-up is essential, especially if medication is the only treatment.
Selective serotonin reuptake inhibitors (SSRIs) are often the first medications prescribed. They work by preventing the reabsorption of serotonin. In general, they are proven as safe and effective with fewer side effects than other types of antidepressants. Examples include sertraline (Zoloft), paroxetine (Paxil), fluoxetine, (Prozac), citalopram (Celexa), and escitalopram (Lexapro).
Serotonin and norepinephrine reuptake inhibitors (SNRIs) work by preventing the reabsorption of serotonin and norepinephrine. Examples are duloxetine (Cymbalta), venlafaxine (Effexor XR), and desvenlafaxine (Pristiq).
Norepinephrine and dopamine reuptake inhibitors (NDRIs) work by preventing the reabsorption of norepinephrine and dopamine. NDRIs like buproprion (Wellbutrin) have less sexual side effects.
Atypical antidepressants do not fit into the other antidepressant categories. Examples are trazodone and mirtazapine (Remeron); both have a sedative effect, so they are taken at bedtime. Vilazodone (Viibryd) is a newer medication available in this category; it has less risk of sexual side effects
Tricyclic antidepressants like imipramine (Tofranil) and nortriptyline (Pamelor) are powerful antidepressants, but the side effects from these medications are greater in number and severity than side effects from newer antidepressants and as such they are the second-line treatment. They are used only if treatment with SSRI medications do not improve symptoms.
Monoamine oxidase inhibitors (MAOIs), the oldest class of antidepressants, like tranylcypromine (Parnate) and phenelzine (Nardil), are only prescribed after all other antidepressants have been tried first and do not relieve symptoms. They have the potential for serious side effects. They are dangerous and even deadly if a strict diet is not followed. They interact with certain foods that contain tyramine, such as wine, cheese, and pickles. The also interact with other medications like decongestants and birth control pills as well as with herbal supplements causing dangerous increases in blood pressure. A newer MAOI called Selegiline (Emsam) is given via a skin patch and has fewer side effects than other MAOIs. They cannot be combined with SSRIs due to the high risk of developing “serotonin syndrome” to the point that if MAOIs are prescribed after an SSRI does not relieve symptoms, there must be at least two weeks between stopping SSRIs and starting MAOIs.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
Military-specific considerations
It is more difficult to notice symptoms of depression in Service members as a result of military culture and the unique challenges and stressors they face. This is particularly true in the initial stages of depression. For example, everyone wears the same uniform and has the expectation of showing good military bearing and maintaining appropriate levels of hygiene, all of which make it difficult to notice subtle changes. In addition, the prevalence of stigma regarding mental health disorders contributes to Service members oftentimes hiding their feelings, withdrawing and disengaging, taking longer to admit to the presence of symptoms and their severity, and waiting longer to seek out help. Consequently, once they do, frequently their depression is more severe.
Service members have military-specific risk factors for and contributors to developing depression, anxiety, and grief disorders, for example, stress injuries from trauma, fatigue, grief, and inner conflict. Trauma from an impact injury after exposure to a toxic event has consequences, including shame, guilt, dissociation, and damage to core beliefs that if not addressed, can develop into a clinical disorder. Operational fatigue, which is considered a wear-and-tear injury can cause symptoms similar to anxiety and depression that become chronic if not addressed. Grief, which is defined as a loss injury, could involve the loss of a fellow Soldier in combat or the loss of who Service members thought they were. Grief increases the risk of developing a clinical disorder, particularly if Service members do not feel the full effects of grief until redeployment. And last, inner conflict, for example losing faith in the mission or leadership, and engaging in behavior inconsistent with their moral code, increases risk of developing a clinical disorder if not addressed in a timely manner. As the number of these mechanisms experienced by Service members increases, the higher the risk of developing a clinical disorder.
Other military specific stressors include mental health stigma, frequent moves and separation from families, and deployment-related trauma and stressors. However, there are protective factors in play as well, such as battle buddies, availability of resources, and a sense of purpose and belongingness. In addition, for those of you who want to talk to someone, but have the legitimate fear that what you say will be repeated to others and/or reported, always remember that your chaplain offers a trusting and confidential environment.
There is another type of depression oftentimes diagnosed in Service members other than Major Depressive Disorder (MDD), Persistent Depressive Disorder (PDD), and mild depression. Adjustment disorder with depressed mood is diagnosed if a Service member develops symptoms of depression within three months of facing a stressor or life problem. Symptoms must cause marked distress and significantly impair daily, social, and occupational functioning.
Diagnosis of TBI and PTSD are both highly associated with a co-diagnosis of depression. Therefore, if you are diagnosed with depression, you should be evaluated for TBI and PTSD as well.
The military uses different screens and measures to evaluate and diagnose depression. Self-report screens/measures include:
The Client Health Questionnaire 2-Item (PHQ-2) is effective for initial screening; a positive screen indicates further evaluation
The Client Health Questionnaire-9 Symptom Checklist (PHQ-9) is a self-report measure that improves diagnostic accuracy and helps with treatment decisions.
The Hamilton Depression Rating Scale (HDRS or HAM-D) is used by clinicians to evaluate the severity of symptoms and response to treatment.
For active-duty Service members, because depression is so treatable, getting a diagnosis will not and should not end your careers; however, there may be changes made to your normal daily duties, at least while you are under treatment.
Always remember that depression is highly treatable, and like any medical condition, the earlier that treatment begins, the better the outcome.
Final thought: Dr. Louise B. Andrew wrote, “Persistent ignorance about depression and misperceptions of it by the public, and even some health providers, as a personal weakness or failing that can be willed or wished away lead to painful stigmatization of and avoidance of the diagnosis by many persons who are affected by the disease.” So, please learn about depression, ask every question you have, take care of yourselves by seeking out help and taking an active role in your care, and please, please, please take care of each other.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
Credible Resources
The sources used for the information in each section were retrieved from American Psychological Association (APA), Anxiety and Depression Association of America (ADAA), Mayo Clinic, Medscape, National Institute of Mental Health, WebMD, and U.S. Department of Veterans Affairs. However, the Matthew Patton Foundation is neither affiliated with nor endorsed by these organizations. Please use the following links for more in-depth information about depression from these organizations.
Depression at http://www.adaa.org/understanding-anxiety/depression and http://www.apa.org/topics/depress/index.aspx and http://www.healthquality.va.gov/guidelines/MH/mdd/
Depression (major depressive disorder) at http://www.mayoclinic.org/diseases-conditions/depression/basics/definition/con-20032977
What is depression (causes, signs & symptoms, who is at risk, diagnosis, treatments, etc) from http://www.nimh.nih.gov/health/topics/psychotherapies/index.shtml
Physiologic factors in depression from http://emedicine.medscape.com/article/805459-overview#aw2aab6b3
Psychodynamic Therapy for Depression from http://www.webmd.com/depression/guide/psychodynamic-therapy-for-depression
What is psychotherapy? From http://www.nimh.nih.gov/health/topics/psychotherapies/index.shtml