Substance Use Disorder (SUD)
This information was obtained from credible government and private organizations and results from evidenced-based medicine; however, it is not meant to replace a medical or psychiatric professional’s advice. It was reviewed by a psychologist who is well-versed in this information and who treats many Veterans. It is current as of March 26, 2015.
What is Substance Use Disorder (SUD)?
Misuse of alcohol and other drugs has been a long-term problem for the military, and their rates of misuse are rising, especially prescription drug misuse. SUD begins with the voluntary act of using a substance that over time becomes compulsive as the person’s ability to choose whether or not to use becomes compromised. This is a result of the effect of prolonged use of a substance on the brain, which affects multiple circuits involved in learning, memory, reward and motivation, and inhibitory control over behavior. This can lead to serious problems with health, relationships, employment and the legal system. SUD is detrimental to discipline, levels of performance, military and family readiness, physical and psychological health and fitness, and the safety of users and everyone around them. SUD is considered a chronic disorder, therefore, the goal of treatment is sustained abstinence and recovery from the multiple consequences SUD incurs. Since illicit drug use in the military is lower than in the civilian population, this section will focus on Alcohol Use Disorder, Opioid Use Disorder and Tobacco Use Disorder.
According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), SUD is the recurrent use of alcohol and/or drugs that causes clinical (meets diagnostic criteria) and significant functional impairment criteria (disability, health problems, inability to meet social, family, occupational, and daily life obligations). A diagnosis is based on presence of risky use, impaired control, social impairment, and pharmacological criteria and is defined as mild, moderate, or severe based on the number of diagnostic criteria the individual meets.
Alcohol Use Disorder (AUD) is the overuse of alcohol that increases risk of accidents, health problems (e.g., liver damage and failure), risk-taking behavior from intoxication that can harm self and others, higher risk of suicide, alcohol withdrawal symptoms, and potential death from alcohol poisoning. There are different levels of drinking, including:
- Moderate Drinking, which is one drink per day for women and two drinks per day for men.
- Binge Drinking, which is drinking five or more drinks in two hours for at least one day in the past 30 days.
- Heavy Drinking, which is five or more drinks on the same occasion for five or more days in a row in the past 30 days.
To meet a diagnosis, AUD specific diagnostic criteria must be met; the number of criteria met determines the severity of AUD—mild, moderate, or severe. Some criteria include:
- Problems controlling the amount of alcohol intake,
- Problems with continuing to use alcohol despite the problems that result from intake (e.g., compulsive behavior)
- Developing tolerance (e.g., needing more and more alcohol to achieve the same level of intoxication over time)
- Engaging in risky situations because of alcohol intake
- Developing withdrawal symptoms when alcohol intake stops
 Opioid Use Disorder is the misuse of opioid drugs, either prescription (e.g., oxycodone - Percocet, hydrocodone – Vicodin) or illicit opioids (e.g., heroin). Many start using prescription opioids for legitimate reasons (e.g., pain relief for an acute injury), but some of the side effects, particularly euphoria (e.g., feeling high, happy, elated, excited) and the feeling of emotional numbness become the primary reason for continuing the use of opioids. Eventually, tolerance develops and the need for more opioids increases, which causes individuals to either increase the dosage (take larger amounts) or decrease the amount of time between doses (take pills more frequently). This can lead to crushing opioid pills to snort or inject, which intensifies euphoria and increases numbness. Eventually individuals may experience physical and psychological dependence, switch to cheaper opioids (e.g., heroin), and have higher risk of both accidental and intentional overdose (suicide). Symptoms of Opioid Use Disorder include:
Opioid Use Disorder is the misuse of opioid drugs, either prescription (e.g., oxycodone - Percocet, hydrocodone – Vicodin) or illicit opioids (e.g., heroin). Many start using prescription opioids for legitimate reasons (e.g., pain relief for an acute injury), but some of the side effects, particularly euphoria (e.g., feeling high, happy, elated, excited) and the feeling of emotional numbness become the primary reason for continuing the use of opioids. Eventually, tolerance develops and the need for more opioids increases, which causes individuals to either increase the dosage (take larger amounts) or decrease the amount of time between doses (take pills more frequently). This can lead to crushing opioid pills to snort or inject, which intensifies euphoria and increases numbness. Eventually individuals may experience physical and psychological dependence, switch to cheaper opioids (e.g., heroin), and have higher risk of both accidental and intentional overdose (suicide). Symptoms of Opioid Use Disorder include:
- Having a strong desire for using opioids as well as inability to control or reduce opioid use
- Continuing to use opioids even though they are interfering with daily life activities, social, familial, and occupational functioning, and fulfilling major obligations
- Looking forward to or obsessing about the next dose
- Developing tolerance and using larger amounts over time
- Spending a lot of time and money to obtain opioids
- Experiencing withdrawal symptoms without the drug (e.g., fever, diarrhea, insomnia, muscle aches, nausea and vomiting, and negative changes in mood)

Tobacco Use Disorder is using any tobacco product. Rates of tobacco use are higher in the military than civilian population. Studies have connected higher use of tobacco among Service members in response to high levels of stress; it is used as a coping mechanism (e.g., multiple deployments and combat exposure increase use of tobacco products and some may start using tobacco during deployment). It is most prevalent in the 18 to 24 year-old age group, those of lower rank, and those with less education. Negative consequences for Service members who smoke include: (a) lower fitness levels and greater risk of physical injury, (b) new or worsened psychological symptoms (e.g., depression symptoms), and (c) damage to nearly every organ, which can lead to stroke, heart disease, respiratory problems, and lung cancer. All can result in premature discharge from service.
After redeployment, Service members face directly opposing situations that can become problematic: adjusting to a non-tobacco culture and finding themselves around Veterans who use tobacco.
The good news is that 7 out of 10 Veterans want to quit and 50% are successful in their efforts, although it can sometimes take more than one attempt.
There are links located in the credible resources section for more in-depth information about the subject matter in this section, including Cannabis Use Disorder, Stimulant Use Disorder, and Hallucinogen Use Disorder.
What are the phases of addiction?
- Experimental use occurs when the substance is first recreationally used, many times as a result of peer pressure.
- Regular use occurs when the substance is taken more often and when users miss school and work, worry about finding more of the substance and losing their connections, disengage from family and friends, spend more time with others who use, and begin to show more tolerance to the drug (e.g., they can handle more of the substance, and therefore, need more of the drug to achieve the same effects).
- Problem or risky use starts when all motivation is lost and the substance becomes more important than anything, including school, work, family, friends, etc. Behavior changes become obvious (e.g., increased secrecy and obvious inability to function in relationships and daily activities). Typically, at this point someone will have noticed the changes and mention them. Substance users may turn to harder substances or begin to sell to support their habit. Legal problems are oftentimes the result.
- Addiction (dependence) occurs when users cannot face daily life without the substance, yet deny they have a problem despite the fact that they have lost control, their social, physical, financial, and legal problems are worse, and they may have thoughts of suicide.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the symptoms of Substance Use Disorders (SUD)?
 In addition to the symptoms listed in the Alcohol Use Disorder, Opioid Use Disorder, and Tobacco Use Disorder sections, users may experience the following:
In addition to the symptoms listed in the Alcohol Use Disorder, Opioid Use Disorder, and Tobacco Use Disorder sections, users may experience the following:
- Confusion
- Violence
- Hostility with confrontation about use
- Making excuses about use
- Decreased appetite and not eating
- Neglecting physical appearance
- Using substances even when alone
- Loss of interest in activities they once enjoyed
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the risk factors for developing Substance Use Disorders (SUD)?
- Stress (e.g., emotional, financial, environmental, chaotic lifestyle)
- Unique military culture
- Deployment
- Distance from support systems

- Relationship strain
- High combat exposure (especially for binge drinking)
- Multiple deployments and combat exposure (highest risk)
- Acute injury, combat-related injury, stress injury (wear and tear) from multiple deployments
- Use of multiple substances (e.g., those using opioids increasingly use alcohol as a supplement)
- Increased use of prescription pain medication after injury that leads to misuse
- Comorbid Diagnoses of depression, TBI, PTSD, sleep disorder
- Damage to the frontal lobe from a TBI (contributes to SUD vulnerability)
- Lack of evidence-based care, particularly for screening and diagnosis
- Genetic tendency
- History of familial substance use
- Prior history of substance use
- Age: 18 to 25 year olds
- Low self-esteem
- Peer pressure
- Access to substances
- Evidence that indicates that young adults move more quickly through the addiction phases
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the barriers to getting help?
- Stigma
- Disconcerting attitudes of others toward those with SUD

- Lack of access to care
- Structure and location of services
- Over reliance on residential care
- Gaps in insurance coverage (e.g., TRICARE restricts services to specific certified facilities that may be geographically distant, doesn’t cover intensive outpatient and office- and community-based services, and does not cover use of some evidence-based medication therapies that are the standard of care)
- Outdated benefit structure and limits
- Current policies (e.g., zero tolerance policy, lack of confidentiality, Command involvement in treatment plan) inhibit care-seeking behavior, thus early diagnosis and treatment*
- Fear of negative consequences/punitive environment (e.g., effect on career, dishonorable discharge and potential criminal prosecution for positive drug test)*
- Shortage of SUD counselors
- Lack of appropriately trained personnel in both SUD and SUD with comorbid conditions
*The Army piloted the Confidential Alcohol Treatment and Education Pilot that proved that when Soldiers were given the opportunity to seek treatment through self-referral, if their SUD was kept confidential and treatment was provided without disciplinary action, they did. This promoted better care, built troop resilience, and encouraged Soldiers to stop hiding the problem and seek care. Please see http://www.army.mil/article/26350/pilot-program-allows-soldier-self-referral-for-alcohol-treatment/ for more information.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
How are Substance Use Disorders (SUD) Screened and Diagnosed?
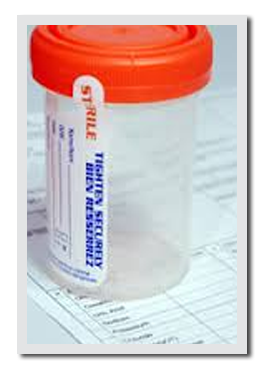
Substance screens through either blood or urine to test for the presence of substances either to confirm initial diagnosis or to monitor treatment compliance. Although blood tests are the better choice for finding a substance and its metabolites, urine screens are oftentimes the test of choice. Be aware that some substances (e.g., opioids) remain in the hair, so your hair can be tested for evidence of long-term use.
 There are self- and clinician-administered questionnaires that screen for the presence of a SUD.
There are self- and clinician-administered questionnaires that screen for the presence of a SUD.
There is a brief confidential self-administer screen called ASSIST on the VA My HealtheVet website that you can take in the privacy of your own home if you suspect you may have a SUD. It will ask you about what substances you have used in the past three months and over your lifetime. Based on your answers, you will be given information about your potential health and other problems based on what you use and the level of use. Your results WILL NOT be stored or sent anywhere. You can print your results for your own records or to bring to your health care provider. The screen is available at the following web address: https://www.myhealth.va.gov/mhv-portal-web/anonymous.portal?_nfpb=true&_pageLabel=mentalHealth&contentPage=mh_screening_tools/ASSIST.HTML&WT.ac=mentalHealth_AssistScreen
Links for the Self-Screening for Illicit Drug Use and Screening for Nicotine Dependence can be found at the following website: http://www.mentalhealth.va.gov/communityproviders/clinic_sud.asp#sthash.3RQe87dF.dpbs
Clinicians use several screens, the positive results of which serve as early warning signs of an SUD and signal the need for further evaluation before problems get worse.
Alcohol Use Identification Test – Alcohol Consumption (AUDIT-C) is a widely used validated screening tool used to asses for alcohol misuse. The AUDIT-C is a three item questionnaire and asks such questions as, “How often did you have a drink containing alcohol in the past week?” A score of four or higher is considered a positive screen and may require further evaluation, with potential for referral and brief intervention depending on evaluation outcomes. A score greater than 7 may indicate dependence and will require further evaluation.
Brief Addiction Monitor (BAM) is a self-report or clinician conducted screening tool used to determine severity of a SUD that generally takes about five minutes to complete. It is used in specialty care settings to support measurement-based treatment. BAM uses 17 items that assess (a) risk factors for SUD, (b) protective factors that support recovery, and (c) drug and alcohol use over the past 30-days. BAM scores can be evaluated in a variety of ways to plan personalized treatment.
More information for ASSIST and BAM is available at the following website: http://www.mentalhealth.va.gov/communityproviders/clinic_sud.asp#sthash.3RQe87dF.dpbs
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What are the treatment options for Substance Use Disorder (SUD)?
It is important to remember that it can be hard to admit to having a SUD and deciding to get help, so providing support to someone who has reached this point is important. Empathy and respect are attributes to employ to help someone with SUD overcome denial and want help; simply saying, “You do not have to do this alone” helps. This lets a person know they are heard, respected, and accepted despite substance use history and the consequences that have resulted from it.
Recovery involves attaining and maintaining abstinence from substance use. Your treatment plan should be individualized and achieved through a variety of ways. Sometimes it may take numerous attempts to achieve recovery. A different treatment may overcome any barriers that prevented prior treatments from working. Therefore, you should be aware of the barriers you might face in achieving recovery because the more aware of them you are, the better you can overcome them. They include:
 Biological factors, such as comorbid disorders (PTSD, TBI) and medical conditions (pain);
Biological factors, such as comorbid disorders (PTSD, TBI) and medical conditions (pain);
Psychological factors, such as low self-esteem, fear of failure, and decreased motivation because you are not fully ready to quit; and
Social factors, such as stigma, lack of resources and sober supports, and living in an environment where there is continued substance use.
So, there are multiple services and effective treatments available to recover from SUD. The types of services used will depend on the specific SUD, presence of polySUD (using more than one substance), and your needs. Not all services will be needed. For those who have become physically dependent on the substance, detox may be the first step and for those who are significantly using, weaning down from, or completely off the substance, may be the first step because it is difficult to engage in therapeutic services while still under the influence. Treatment for withdrawal will be followed by a personalized treatment and relapse prevention plan to improve your ability to recover. Other factors that increase the chances of recovery include:
- taking responsibility for your own recovery
- focusing on yourself as a whole person considering your environment and mind-body connection (biopsychosocial model)
- being actively involved in the treatment process and plan
- avoiding environments and people who use
- involving family and friends depending on the nature of the relationship (e.g., family and friends whom you may have alienated because of your substance use may be less supportive),
- recognizing that recovery takes time, while still celebrating small successful changes
If you suffer from a comorbid condition (PTSD, TBI, depression), you must advocate for yourself and receive treatment for any and all of these conditions at the same time. Evidence-based medicine is very clear on this; in order for you to fully recover, you must receive treatment for any comorbid conditions.
Therapy with or without medication
Inpatient and residential settings: Long-term residential treatment lasting six to 12 months is relatively uncommon and is reserved for those with severe SUD. For example, therapeutic communities (TC) are highly structured programs that use a community-treatment approach involving both the treatment staff and those seeking recovery as the agents of change to achieve resocialization to a SUD-free lifestyle. Short-term in-house treatment is more common and usually involves detoxification (medically managed withdrawal) and providing the initial intensive treatment (e.g., co-treatment for depression or PTSD) in preparation for outpatient treatment.
Individual and group counseling: The focus of counseling for individuals is reducing or stopping substance use, building skills (e.g., communication and problem-solving skills), adhering to the treatment/recovery plan, and achieving good individual, social, family, educational, and occupational outcomes. The focus of group counseling, which is oftentimes used in conjunction with individual counseling, is to provide social reinforcement to aid recovery. Each form of counseling will be tailored for specific populations. Counselors will assess, plan treatment, and work toward helping an individual achieve recovery using a variety of therapies.
Cognitive Behavior Therapy (CBT) helps users to recognize and stop negative patterns of thinking and behavior that lead to SUD, such as identifying the stressors, feelings, and situations that lead to substance use so they avoid these situations (e.g., people who use, places they used) with the goal of helping them abstain from substance use. You will find a more detailed description of CBT in the treatment of depression section.
Motivational enhancement therapy aka motivational interviewing will make the most of users’ readiness to change behavior and exercise free choice to enter treatment by building on your intrinsic motivation and commitment to specific plans for treatment and recovery. Both you and your therapist develop a collaborative partnership wherein you are viewed as valuable and self-worthy and that you both bring knowledge to the table.
Contingency management aka motivational incentives uses positive reinforcement (incentives) to encourage users to reinforce positive behaviors, such as maintaining abstinence. The evidence-base shows that contingency management is clearly the most powerful and flexible of the therapies available for substance use, yet it has very low acceptance across the clinical community because of (a) the high cost of incentives and (b) lack of support for implementation from top-down administrators.
Family therapy involves the family to address a range of factors that influence a family member’s substance use and improve overall family functioning. The involvement and support of family increases chances of achieving and maintaining recovery.
12-step facilitation therapy like Alcoholics and Narcotics Anonymous use group settings to guide and support your recovery from SUDs.
Medications
Medications for SUD, called Medication-Assisted Treatment (MAT), are used to reestablish normal brain function and manage symptoms of withdrawal—hunger, cravings, anxiety, depression, insomnia, irritability, restlessness, and difficulty concentrating—as well as cope with the urge to use again by blocking reward sensations and inducing negative feelings and sensations when a substance is used.
Medications for treatment of alcohol misuse
There are three FDA approved medications for Alcohol Use Disorder (AUD), with a promising fourth medication (topiramate) in clinical trials. Naltrexone, used for treatment of Opiate Use Disorder (OUD) is also used for AUD because the same receptors are involved. For AUD, naltrexone blocks the rewarding effects of and cravings for alcohol as well as reduces relapse for those who are heavy users of alcohol. It is more helpful for some than others, which scientists believe is related to genetic differences. Acamprosate reduces symptoms of prolonged withdrawal (e.g., anxiety, insomnia, sadness, anguish, restlessness, irritability, depression, and dissatisfaction) and tends to be more effective for those with severe dependence. This medication has been proven effective in helping users who have achieved abstinence to maintain it for long periods of time (e.g., weeks to months). Disulfiram prolongs the breakdown of alcohol, so the byproduct, acetaldehyde, accumulates. This produces an unpleasant reaction including flushing, nausea, vomiting, and palpitations (you can feel your heart beating) when the user drinks alcohol. This medication is very useful for those who are highly motivated to stop drinking.
Medications for treatment of opioid misuse
There are three medications used to treat OUD. Methadone and buprenorphine work by acting on the same part of the brain that opiates do to decrease withdrawal symptoms and relieve cravings, whereas extended-release injectable naltrexone blocks the effects of opioids at receptor sites, thus reducing withdrawal symptoms and cravings. Naltrexone is used only after detox is completed, but because of compliance problems, it is not the first medication of choice. All three medications help users stop drug seeking behavior and help them engage in behavioral treatments with greater success.
Relapse occurs when a person who has successfully abstained from substance use begins to use again. This is an important time wherein the support this person receives sends the message that he or she made a mistake that can be fixed by abstaining again versus he or she has failed and cannot succeed at maintaining sobriety. Empathetic support to help get the person back on the road to recovery is essential.
Treatment specifically for tobacco cessation
Evidence-based treatment for smoking cessation involves using FDA-approved medication and tobacco cessation counseling.
Types of medication
Nicotine Replacement Therapy (NRT) from Nicotine patch, gum, and lozenges provides replacement nicotine to reduce withdrawal symptoms without the harmful ingredients found in tobacco. You can use one type or a combination of two types(e.g., patch for consistent dose for withdrawal relief with either gum or lozenges to control cravings). You can get a nicotine inhaler or nasal spray via prescription as well.
Bupropion (Zyban) is a prescription medication that reduces the urge to smoke; is does not contain nicotine. You should start this medication one to two weeks prior to your quit date. It can be combined with one NRT (e.g., nicotine gum or lozenge).
Varenicline (CHANTIX) is a prescription medication that blocks the effect of nicotine in the brain the result of which makes smoking less enjoyable and reduces withdrawal; it noes not contain nicotine. You should start this medication one to two weeks prior to your quit date. You CANNOT combine this medication with any other smoking cessation medication.
For more information regarding Smoking Cessation Medications, please visit http://www.publichealth.va.gov/smoking/quit/counseling.asp
Tobacco Cessation Counseling
Since counseling along with medication has been shown by evidenced-based medicine to be the most successful way to quit smoking, please see Tobacco Cessation Counseling at http://www.publichealth.va.gov/smoking/quit/counseling.asp for more information about what the VA has to offer.
*Having the support of family and friends contributes to quitting successfully. It may take several attempts to quit for good, up to five or six times. But it can be done especially if you know why you want to quit.
The National Cancer Institute provides free, accurate, and evidence-based information and professional assistance to help support the immediate and long-term needs of people trying to quit smoking. See http://smokefree.gov The National Cancer Institute is part of the National Institutes of Health under the purview of the U.S. Department of Health & Human Services.
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
What can leadership at all levels do?
The Department of Defense (DoD) recently authorized the Institute of Medicine (IOM) to examine current military-wide policies and procedures in regard to prevention, screening, diagnosis, treatment, and follow-up of/for SUDs. The results indicate that many current practices are outdated and ineffective. This is very similar to the IOMs evaluation of health care practices in the late 90’s that showed that thousands of patient deaths per year were deemed preventable and caused by medical errors from lack of quality care. The report “To Err is Human” called for use of evidence-based care and use of performance measures to monitor and evaluate care, which sparked the quality care movement we see today. Just like with health care, the IOM listed recommendations for the DoD to use evidence-based interventions and monitor and evaluate outcomes (performance measures) for SUDs. Although it is the DoDs responsibility to enact military-wide change, there are ways for leaders at all levels to create change. This is particularly true since some medical decision-making has been placed under the purview of Command.
Leaders can continue or begin to:
- Learn about and support research examining the causes of substance use, prevention, screening, diagnosis, treatment, and especially, follow-up
- Adopt and implement known evidence-based care for prevention, routine screening, diagnosis, and provision of effective treatment, such as using multidisciplinary treatment teams, emphasizing out-patient services, using group therapy, taking advantage of computer-assisted
 Cognitive Behavioral Training (CBT)
Cognitive Behavioral Training (CBT) - Update command-level policies and practices to increase access to care and use of evidence-based care
- Develop and follow guidelines for referral to specialty providers
- Develop and follow mechanisms to support interventions
- Monitor and evaluate interventions for effectiveness (performance measures)
- Understand that follow-up is essential; ensure follow-up is provided
- Allow Services members to remain in contact with their counselors for as long as necessary; do not take users out of treatment before the entire course of treatment is complete
- Reduce stigma that prevents Service members from seeking care for SUDs
- Ensure that there are options available for confidential treatment of SUDs*
- Educate Service members about the risks associated with excessive alcohol consumption and drug use (e.g., DUIs), and binge drinking with the goal of reducing their incidence
- Use various methods for education (e.g., less PPTs, more interaction)
- Be proactive and attack the problem before it starts by limiting access to alcohol and certain medications, otherwise
- Enforce routine screening
- Enforce underage drinking laws
- Recognize medication-seeking behaviors without ignoring and undertreating physical pain
- Monitor prescribing trends before dispensing medications that have potential for abuse (Army pharmacists are monitoring Soldiers’ medication when they are using multiple prescriptions)
- Continue limiting duration for opioid prescriptions to six months
*Read about the Army’s Confidential Alcohol Treatment and Education Pilot Program here http://www.army.mil/article/26350/pilot-program-allows-soldier-self-referral-for-alcohol-treatment/
There are links located in the credible resources section for more in-depth information about the subject matter in this section.
Credible Resources
The sources used for the information in each section include American Psychological Association (APA), Community Provider Toolkit, Institute of Medicine (IOM), Making the Connection, MedlinePlus, Mental Health Substance Abuse and Mental Health Services Administration (SAMHSA), National Cancer Institute (NCI), National Institute on Drug Abuse (NIDA), National Institutes of Health (NIH), U.S. Department of Health & Human Services (HSS), and U.S. Department of Veterans Affairs. However, the Matthew Patton Foundation is neither affiliated with nor endorsed by these organizations. Please use the following links for more in-depth information about SUDs from these organizations.
Assessing for a Substance Use Problem from http://www.mentalhealth.va.gov/communityproviders/clinic_sud.asp#sthash.3RQe87dF.dpbs
Confidential Alcohol Treatment and Education Pilot Program from http://www.army.mil/article/26350/pilot-program-allows-soldier-self-referral-for-alcohol-treatment/
Substance Use from http://www.mentalhealth.va.gov/substanceabuse.asp
Substance Use Disorders from http://www.samhsa.gov/disorders/substance-use and http://www.nlm.nih.gov/medlineplus/ency/article/001522.htm
Substance Use Disorders in the U.S. Armed Forces from http://www.iom.edu/Reports/2012/Substance-Use-Disorders-in-the-US-Armed-Forces.aspx
Substance Abuse in Military Life from http://www.drugabuse.gov/related-topics/substance-abuse-in-military-life
Drug Facts: Substance Abuse in the Military from http://www.drugabuse.gov/publications/drugfacts/substance-abuse-in-military
Making the Connection –shared experiences and support for Veterans at http://maketheconnection.net/
The following link will take you to the website that provides easy-to-understand information on SUD and provides personal stories from Active-duty Soldiers, Veterans, family members, National Guard and Reserve etc. as well as multiple links that help you learn about and find treatment options that will best serve you; http://maketheconnection.net/symptoms/alcohol-drug-problems
You can find s SUD program near you using the a VA locator at http://www.va.gov/directory/guide/SUD_flsh.asp?isFlash=1
Tobacco and Health from http://www.publichealth.va.gov/smoking/index.asp
Other Resources from the VA including Information resources, mutual help organizations (e.g., AA, NA) and Support for family and friends are located at http://www.mentalhealth.va.gov/substanceabuse.asp
The Department of Health & Human Services provides one-stop access to U.S. Government information on tobacco from its various operating and staff divisions at http://betobaccofree.hhs.gov/index.html
The U.S. Department of Veterans Affairs offers its Smoking Quitline the use of which doubles your chance of quitting smoking versus getting no support at all. Any Veteran receiving health care through the VA is eligible to use this quitline. See http://www.publichealth.va.gov/smoking/quitline.asp for more information.
You can also get information about Tobacco Cessation Counseling at http://www.publichealth.va.gov/smoking/quit/counseling.asp and information on smoking cessation medications at http://www.publichealth.va.gov/smoking/quit/counseling.asp